Each year, employees miss work and potential wages
due to work-related musculoskeletal disorders (MSDs). According to the Bureau
of Labor Statistic (BLS), 335,390 American workers experienced MSDs serious
enough to require time off work in 2007.
In fact, injuries to the muscles and skeleton are
among the most common lost time illnesses and injuries in virtually every
industry.
Musculoskeletal disorders occur when there is a
mismatch between what your job requires you to do and what your body is capable
of doing. MSDs can affect worker in job activities across many diverse
workplaces and tasks.
The Institute of Medicine estimates that the
economic burden of MSDs in the workplace, as measured by compensation costs,
lost wages, and lost productivity, are between $45 and $54 billion annually. Historically,
overexertion, one form of MSDs, is the number one cause of workplace injury.
In 2007, there were 1,2 million MSD cases requiring
days away from work in private industry out of 4 million total recordable
cases. Of these, 335, 390 cases required an average of nine days away from work,
two more days than the average for all days away from work cases.
Because of statistics like these, ergonomics has
become an important and serious issue for industry.
The term “ergonomic” is derived from two Greek
words: “erg” meaning work and “nomas” meaning natural laws.
Basically, ergonomics is the science of adjusting
job conditions, equipment, and tasks to match the body’s natural ways of
functioning.
The goal of ergonomics is to prevent illness and
injury, assure high productivity, and promote satisfaction in the workplace.
In the absence of a federal ergonomics standard, the
Occupational Safety and Health Administration (OSHA) has addressed ergonomics
in the workplace under the authority of section 5 (a)(1) of the Occupational
Safety and Health Act.
This section is referred to as the General Duty
Clause and requires employers to provide work and a work environment free from
recognized hazards.
Many employers have realized that the implementation
of an ergonomics program is in their best interest for the reduction of
injuries and illnesses.
An ergonomics program addresses some basic elements
such as employers and employee responsibilities, hazards identification and
information, job hazard analysis and control, training, medical management,
records, and programs evaluation.
Your company’s ergonomics programs is designed to
help keep you healthy, productive and motivated while making your working life
as enjoyable as possible.
Your company can express its commitment in a variety
of ways. These include holding employee meeting to discuss ergonomics operational
goals and priorities that are firm, achievable, and in line with cost
reduction, productivity, and quality initiatives.
In addition, your employer may commit resources to
training, administrative needs, expertise, and ergonomics improvements or issue
policy statements that define support and cooperation from management,
supervision, and employees.
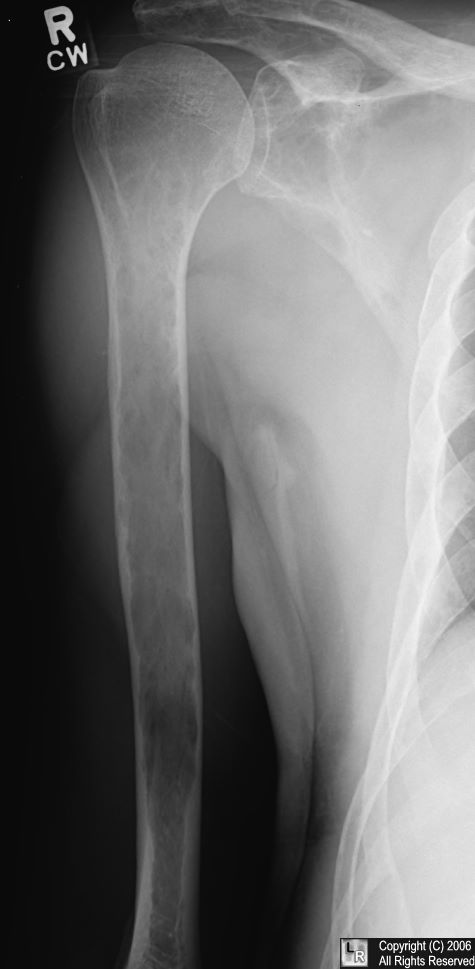
Musculoskeletal Disorders (MSDs) definitions: Are
disorders of the muscles, ligaments, tendons, cartilage, joints, nerves, or
spinal discs that have been diagnosed by physical exam, medical history, or
specific medical test.
They typically result from gradual or chronic development,
as opposed to an acute event or injury caused by, for example, a slip or fall.
MSDs like carpal tunnel syndrome have very distinct signs and symptoms. Other disorders,
such as lower back pain, are simply defined by the location of the pain.
To better understand ergonomics, you should be
familiar with the major parts of the musculoskeletal system:
Ø Bones:
Provide structural support and are connected to one another at joints, which
allow movement between body segments.
Ø Muscles:
Contract and shorten, causing movement, just contract to provide stability. The
respiratory and circulatory systems supply nutrients and oxygen necessary for movement
of muscles.
Ø Ligaments
and tendons: ligaments connect bone to bone and provide stability at the
joints, while tendons attach muscle to the bone.
Ø Cartilage:
Provides the joints with low friction surface that help with movement.
Ergonomics Awareness
Recognizing the early signs and symptoms of injuries
to the muscles and skeleton and reporting them as soon as possible is very
important. A health care provider (HCP) can observe the signs. Symptoms,
however, are subjective and a patient needs to report them to HCP.
Signs of injury to the muscles and skeleton include
redness or loss of color, swelling, loss of function, deformity such as a lump,
decreased range of motion, and decreased grip strength.
Symptoms are your body’s way of warning you that you
may be developing an injury. Symptoms of injury to the muscles and skeleton can
vary in severity, depending on the amount of your exposure.
Eventually the symptoms become more severe as
exposure continues and will appear even after rest. The pain may increase to a
point where it becomes difficult to perform your work or even to a point where
you are unable to perform any physical work activities.
Examples of symptoms of injury to the muscles and
skeleton include numbness, burning, tingling, aching, pain or soreness,
stiffness, and cramping.
Early reporting is vital in preventing or minimizing
injury to the muscles and skeleton. As an employee, you must feel free to
report any signs or symptoms of physical discomfort as soon as possible to your
supervisor or other personnel, such as a plant nurse or HCP.
Employers can also gather information by conducting
symptoms surveys and interviews.
Risk Factors
The OSHA has identified a high rate of injury among
workers in various industries. It is impossible to determine the exact weight
lifted or the number of repetition that will either cause or prevent injury.
However, establishing a systematic approach to
address such issues as repetition, excessive force, awkward posture, and heavy
lifting reduces the chance that you may ne injured.
Identifying risk factors in the workplace, before
injuries to the muscle and skeleton are discovered, is an important step in
keeping you healthy.
Your employer can use several methods to detect risk
factors, such as interviews with workers and supervisors, and walk-through
observations of the workplace.
A more formal approach would be to use a
standardized checklist to evaluate job tasks against risk factors.
There are many different types of risk factors for
injuries to the muscle and skeleton, some of which are not entirely
work-related.
Risk factors for work-related musculoskeletal disorders
are cumulative and can include off-work activities as well. Physical limitations,
previous injuries, or existing health problems can contribute to increased
risk.
It is often difficult to determine the impact that
work activities versus non-work activities (sport or medical conditions such as
rheumatoid arthritis, diabetes, and thyroid conditions) have on the disorder.
For example, in the general population, non-work
causes of lower back pain are probably more common than workplace causes.
When jobs have risk factors in combinations and high
levels, the risk of developing a musculoskeletal disorder will increase. The level
of risk also depends on the intensity, frequency, and duration of exposure. Examples
of risk factors include repetitive, forceful, or prolonged exertion and
pushing, pulling, or carrying heavy objects.
Risk factors (Actions)
·
Repetitive, forceful, or prolonged
exertion
·
Frequent or heavy lifting
·
Pushing, pulling, or carrying of heavy
objects
·
Prolonged awkward postures
·
Work in the cold
·
Insufficient pauses and rest breaks for
recovery
Risk factors (Conditions)
·
Contact stresses
·
Machine-paced work
·
Stress
·
Unfamiliar or unaccustomed work
·
Vibration
Gathering data is a vital step toward the
identification of a problem. Checklists can be used to provide the initial
identification of a job or task which may put a worker at risk for developing
an injury to the muscles or skeleton.
It is important to understand that the checklist
findings must be viewed as a whole to determine if the individual problems
suggest the same underlying root cause.
Control Methods
Many employers provide engineering controls, such as
lift-assist equipment, that go unused or under-used as the employees hurry to
complete their tasks.
Engineering controls reduce or eliminate the
condition by modifying or redesigning workstations, environmental conditions,
tools and equipment, processes, or materials.
For instance, a situation was reviewed in the
electrical industry, where tasks included hammering, crimping, wrapping,
winding, soldering, painting, and various electric motor assemble operations.
Problem: risk factor involved in these types of
tasks included repetitive and forceful exertions, awkward postures, and contact
stress. Workers were found to suffer from upper limb and neck illnesses and
injuries.
Solutions: included raised standing surfaces, a
modified mallet handle, and low force clamps. Job rotation, training programs,
and early reporting were also needed.
Workstation should be adjustable to fit your body. Furniture
and equipment should be positioned to prevent excessive twisting, reaching, and
leaning.
Eyes: Computer monitors should be placed so that the
top of the screen is just below eye level.
Arms and back: Chair should have adjustable armrests
to take the load off your neck and shoulders. Chair should have back rests that
fit your back.
Knees and feet: Chair should ne adjustable to allow
your knees to be bent at a right angle. Chair should be adjustable to allow
your feet to rest flat on the floor. Footrest may be used.
When your finger are on the keyboard, your wrist
should be straight in a neutral position with the upper arm vertical and the
forearm at a 90 degree angle to the upper arm.
Your shoulders should be relaxed and your elbows
close to your sides. Reclining and reaching should also be avoided.
When using the mouse, you should be able to maintain
the correct arm and wrist position. The mouse should be at the same levels as
the keyboard and the same distance from your body as the keyboard.
Administrative controls are changes in the workplace
that adjust work practices, procedures, and management policies.
Specific examples include rest breaks, alternative
tasks, slower work pace, redesign of work methods, and employee rotation.
Consider his example of an office work setting. Management
reviewed an office environment that involved primarily data entry and tasks
involving video display units.
Problems: risk factors identified from these tasks
included repetitive exertions, awkward postures, glare, and poor illumination. Personnel
experienced problems with upper limbs, neck, back, and eyestrain.
Solutions: included reduction glare and improving
workstation design. A vision test program and a rest break schedule where also
suggested.
You would use personal protective equipment (PPE),
such as gloves, to reduce vibration and prevent injury.
Always use engineering control s first if possible,
followed by administrative controls. Use PPE only as a last resort.
Studies show that wearing a back belt does not
reduce injury rates or the number of lost work days. However, wearing a back
belt and having training on lifting techniques may reduce lost work days for
people who have had lower back pain in the past.
Because musculoskeletal disorders involving the back
are among the most costly occupational injuries, it is important to review back
safety and some basic techniques for prevention of back injuries.
These techniques include good posture, proper
lifting, and the practice of basic exercises, such as stretching.
To evaluate your posture, stand with your back
against a doorframe and slip your hand between the doorframe and the small of
your back. Your hand should slide in easily and slightly touch your back and
the doorframe.
When possible, plan jobs to avoid unnecessary
lifting. Improper lifting, especially when combined with twisting, is the most
common way to injure your back.
Correct posture: Place feet firmly apart with one
foot forward for stability. Bend at the knees (not at the waist) and keep your
back as close to vertical as possible.
Incorrect posture: two of the most common mistake
made when lifting are bending at the waist instead of the knees and holding the
load too far out in front of you.
When lifting, tighten your stomach muscle as soon as
you lift to support your spine, breathing out as you lift. Do not hold your
breath.
Remember t use your leg muscles instead of your back
muscle to lift the load. Do not twist your body while lifting and keep the load
close to your body as you lift.
The best path to a healthy back is to control your
weight, exercise, and reduce back stress caused by lifting or poor posture.
Excessive upper body weight such as potbelly
contributes to poor back posture and back pain because of the added stress
placed on the components of the back.
A regular exercise program that includes flexibility
and strengthening exercises can help prevent injury or re-injury to your back.
Consult your healthcare provider before beginning an exercise program.
Remember to report signs, symptoms, and hazards of
MSDs and make recommendations on appropriate ways to control them. Ways to make
these recommendations include e-mail, letters, and notes to your supervisor.
Recommendations can also be made verbally through an
employee representative or by serving on health and safety committees. Always follow
applicable workplace procedures and safety and health rule.
Summary:
Employers are not the only ones with specific
responsibilities. You, as an employee, have an important role also.
Your responsibilities include:
v Recognizing
the signs and symptoms of MSDs and the value of reporting them early
v Identifying
MSD hazards in your job
v Knowing
how to use and evaluate the control measures your employers implements, and
v Working
in ways that will reduce the risks in your job
Retrieved from: http://berryplastics.skillport.com/skillportfe/main.action?content=myprogressNew